SOURCE: Mayo Clinic
Lung Cancer
Diagnosis
Testing healthy people for lung cancer
People with an increased risk of lung cancer may consider annual lung cancer screening using low-dose CT scans. Lung cancer screening is generally offered to people 55 and older who smoked heavily for many years and are otherwise healthy.
Discuss your lung cancer risk with your doctor. Together you can decide whether lung cancer screening is right for you.
Tests to diagnose lung cancer
If there’s reason to think that you may have lung cancer, your doctor can order a number of tests to look for cancerous cells and to rule out other conditions.
Tests may include:
- Imaging tests. An X-ray image of your lungs may reveal an abnormal mass or nodule. A CT scan can reveal small lesions in your lungs that might not be detected on an X-ray.
- Sputum cytology. If you have a cough and are producing sputum, looking at the sputum under the microscope can sometimes reveal the presence of lung cancer cells.
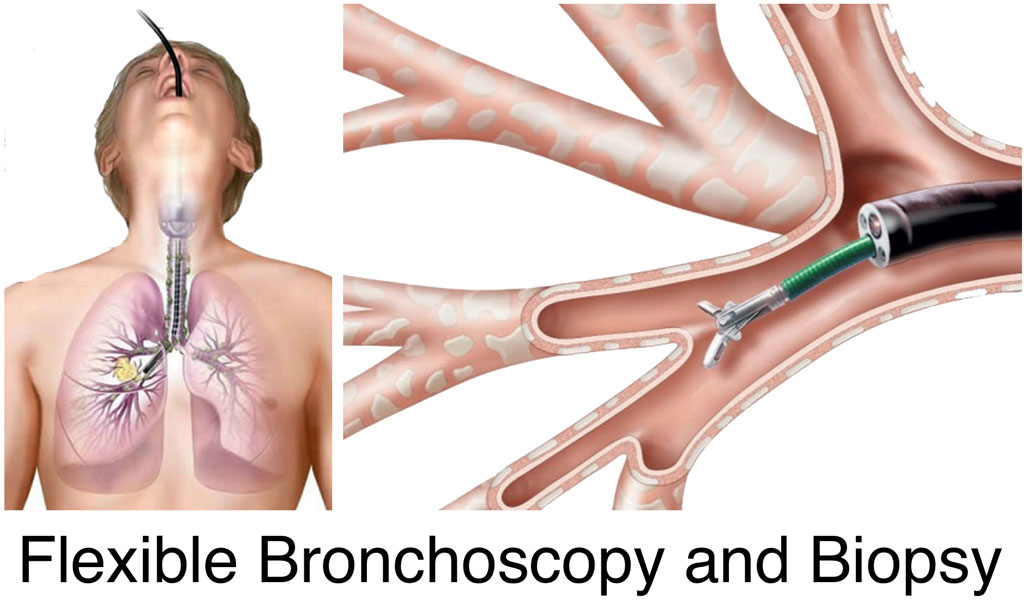
- Tissue sample (biopsy). A sample of abnormal cells may be removed in a procedure called a biopsy. Your doctor can perform a biopsy in a number of ways, including bronchoscopy, in which your doctor examines abnormal areas of your lungs using a lighted tube that’s passed down your throat and into your lungs; mediastinoscopy, in which an incision is made at the base of your neck and surgical tools are inserted behind your breastbone to take tissue samples from lymph nodes; and needle biopsy, in which your doctor uses X-ray or CT images to guide a needle through your chest wall and into the lung tissue to collect suspicious cells. A biopsy sample may also be taken from lymph nodes or other areas where cancer has spread, such as your liver.
Careful analysis of your cancer cells in a lab will reveal what type of lung cancer you have. Results of sophisticated testing can tell your doctor the specific characteristics of your cells that can help determine your prognosis and guide your treatment.
Tests to determine the extent of the cancer
Once your lung cancer has been diagnosed, your doctor will work to determine the extent (stage) of your cancer. Your cancer’s stage helps you and your doctor decide what treatment is most appropriate.
Staging tests may include imaging procedures that allow your doctor to look for evidence that cancer has spread beyond your lungs. These tests include CT, MRI, positron emission tomography (PET) and bone scans. Not every test is appropriate for every person, so talk with your doctor about which procedures are right for you.
The stages of lung cancer are indicated by Roman numerals that range from 0 to IV, with the lowest stages indicating cancer that is limited to the lung. By stage IV, the cancer is considered advanced and has spread to other areas of the body.
More Information
Treatment
You and your doctor choose a cancer treatment plan based on a number of factors, such as your overall health, the type and stage of your cancer, and your preferences.
In some cases, you may choose not to undergo treatment. For instance, you may feel that the side effects of treatment will outweigh the potential benefits. When that’s the case, your doctor may suggest comfort care to treat only the symptoms the cancer is causing, such as pain or shortness of breath.
Surgery
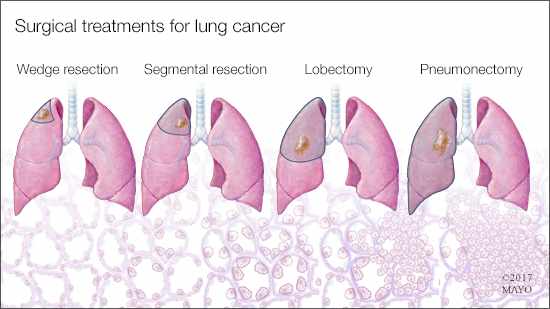
During surgery your surgeon works to remove the lung cancer and a margin of healthy tissue. Procedures to remove lung cancer include:
- Wedge resection to remove a small section of lung that contains the tumor along with a margin of healthy tissue
- Segmental resection to remove a larger portion of lung, but not an entire lobe
- Lobectomy to remove the entire lobe of one lung
- Pneumonectomy to remove an entire lung
If you undergo surgery, your surgeon may also remove lymph nodes from your chest in order to check them for signs of cancer.
Surgery may be an option if your cancer is confined to the lungs. If you have a larger lung cancer, your doctor may recommend chemotherapy or radiation therapy before surgery in order to shrink the cancer. If there’s a risk that cancer cells were left behind after surgery or that your cancer may recur, your doctor may recommend chemotherapy or radiation therapy after surgery.
Radiation therapy
Radiation therapy uses high-powered energy beams from sources such as X-rays and protons to kill cancer cells. During radiation therapy, you lie on a table while a machine moves around you, directing radiation to precise points on your body.
For people with locally advanced lung cancer, radiation may be used before surgery or after surgery. It’s often combined with chemotherapy treatments. If surgery isn’t an option, combined chemotherapy and radiation therapy may be your primary treatment.
For advanced lung cancers and those that have spread to other areas of the body, radiation therapy may help relieve symptoms, such as pain.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. One or more chemotherapy drugs may be given through a vein in your arm (intravenously) or taken orally. A combination of drugs usually is given in a series of treatments over a period of weeks or months, with breaks in between so that you can recover.
Chemotherapy is often used after surgery to kill any cancer cells that may remain. It can be used alone or combined with radiation therapy. Chemotherapy may also be used before surgery to shrink cancers and make them easier to remove.
In people with advanced lung cancer, chemotherapy can be used to relieve pain and other symptoms.
Radiosurgery
Stereotactic body radiotherapy, also known as radiosurgery, is an intense radiation treatment that aims many beams of radiation from many angles at the cancer. Stereotactic body radiotherapy treatment is typically completed in one or a few treatments.
Radiosurgery may be an option for people with small lung cancers who can’t undergo surgery. It may also be used to treat lung cancer that spreads to other parts of the body, including the brain.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
Many targeted therapy drugs are used to treat lung cancer, though most are reserved for people with advanced or recurrent cancer.
Some targeted therapies only work in people whose cancer cells have certain genetic mutations. Your cancer cells may be tested in a laboratory to see if these drugs might help you.
Immunotherapy
Immunotherapy uses your immune system to fight cancer. Your body’s disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that blind the immune system cells. Immunotherapy works by interfering with that process.
Immunotherapy treatments are generally reserved for people with advanced lung cancer.
Palliative care
People with lung cancer often experience signs and symptoms of the cancer, as well as side effects of treatment. Supportive care, also known as palliative care, is a specialty area of medicine that involves working with a doctor to minimize your signs and symptoms.
Your doctor may recommend that you meet with a palliative care team soon after your diagnosis to ensure that you’re comfortable during and after your cancer treatment.
In one study, people with advanced non-small cell lung cancer who began receiving supportive care soon after their diagnosis lived longer than those who continued with treatments, such as chemotherapy and radiation. Those receiving supportive care reported improved mood and quality of life. They survived, on average, almost three months longer than did those receiving standard care.